Lichen planopilaris

What is Lichen Planopilaris?
Lichen planopilaris (LPP) is a form of alopecia (hair loss) which can be cicatricial (scarring) and permanent in nature. While the cause is unknown, it is likely a primary inflammatory process induced by genetic and/or environmental factors, rather than secondary to infections, burns, surgical scars, caustic hair products, etc. Thus, it is a disease centered around the follicular unit itself.
There are three major variants of LPP that are distinguished primarily by clinical pattern of involvement: classic, frontal fibrosing alopecia (FFA), and Graham-Little-Piccardi-Lasseur syndrome (GLPLS).
Symptoms & Causes
The exact cause of Lichen Planopilaris (LPP) isn't fully understood, but it appears to be related to immune system problems. In LPP, immune cells called lymphocytes attack a part of the hair follicle called the "bulge," which contains stem cells essential for hair growth. When these stem cells are destroyed, it results in permanent hair loss.
This immune attack could be triggered by factors like drugs or viruses attaching to hair follicles. Another possibility is that the immune system mistakenly identifies hair follicles as foreign invaders and attacks them. Some people with LPP have genetic differences in a protein called "MHC class I," which helps the immune system distinguish between the body's own cells and foreign ones. In these individuals, the immune system fails to recognize hair follicles as part of the body and destroys them.
Additionally, researchers have discovered that some individuals with a related condition called Graham-Little-Piccardi-Lassueur Syndrome (GLPLS) have antibodies against a protein called "INCENP," which plays a role in cell division and hair growth.
Recent studies have shown that people with LPP have lower levels of a protein called "PPAR gamma." This protein is important for maintaining healthy hair follicles and sebaceous glands (glands that produce oil for the hair). When PPAR gamma levels are low, it can lead to sebaceous gland problems and a buildup of harmful lipids, triggering the immune system to attack the glands and nearby stem cells.
Besides immune issues, hormones also seem to play a role in LPP, especially since it often affects postmenopausal women and can respond to treatments that block androgens (male hormones).
LPP mostly affects middle-aged women but can also occur in men, young adults, and, rarely, children. It is more common in people with lighter skin tones compared to those with darker skin. There is also an association between LPP and hypothyroidism (underactive thyroid) (Wikipedia) (Acronym Finder).
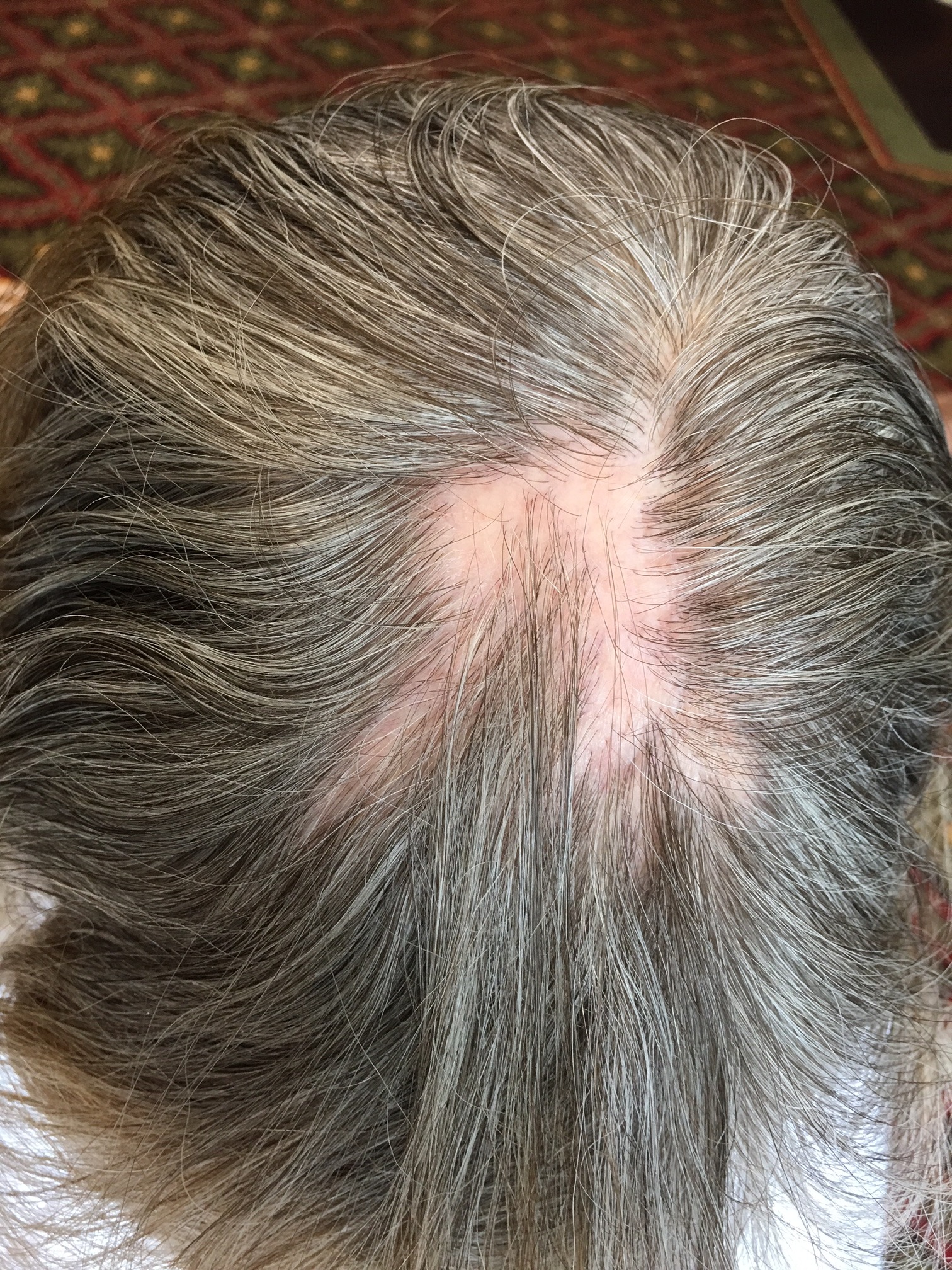
Classic Lichen Planopilaris (LPP) usually affects the top (vertex) and sides (parietal regions) of the scalp, while Frontal Fibrosing Alopecia (FFA) appears in a band-like pattern, 1-8 cm wide, across the front and sides of the scalp. FFA also often affects the eyebrows. Graham-Little-Piccardi-Lassueur Syndrome (GLPLS) involves a combination of LPP, non-scarring hair loss in the armpits and pubic area, and a lichenoid follicular rash. There is also a diffuse pattern variant of LPP, which results in widespread hair thinning.
These three main types of LPP share common early signs: redness and scaling around hair follicles, which eventually lead to permanent scarring hair loss. These symptoms are most noticeable around the edges of hair loss patches, indicating active disease. Initially, these patches may be small and scattered but can merge into larger areas with no visible hair follicles. Symptoms like itching, burning, and scalp tenderness are common, along with possible skin, nail, mouth, or genital issues. Cutaneous lichen planus typically appears as itchy, purple, flat-topped bumps on the skin.
The progression of LPP varies greatly; it can develop quickly or slowly over many years, with hair loss being patchy or widespread. Some people may experience periods of heavy hair shedding during active phases of the disease, while others may have times of remission when the disease is inactive.
It is important to inform your dermatologist if you experience rashes, mouth sores, or genital sores along with hair loss, as these can be related to lichen planus.
Diagnosis & Treatments

To diagnose scarring hair loss such as Lichen Planopilaris (LPP), a detailed history, thorough scalp and skin examination, and appropriate lab tests are essential. A scalp biopsy is also critical and often performed to confirm the diagnosis. Early diagnosis and treatment can help prevent permanent hair follicle damage. Once diagnosed, your dermatologist will create a tailored treatment plan.
The goal of treatment is to stop the inflammation to minimize permanent hair loss. Treatment effectiveness varies, but early signs of the disease usually respond better to treatment than advanced stages. Active LPP signs include ongoing hair loss, redness, scaling on the scalp, itching, inflammation, and an inflammatory infiltrate on biopsy.
Mild cases may be managed with topical corticosteroids and anti-inflammatory shampoos like tea tree oil. For more severe or localized cases, corticosteroid injections may be added. For widespread or severe cases, oral corticosteroids or hydroxychloroquine might be used. If these treatments are ineffective, immune suppressant drugs like azathioprine, mycophenolate mofetil, or cyclosporine may be necessary. Other treatments that have shown effectiveness include tetracyclines, griseofulvin, minoxidil, naltrexone, and the 308 nm excimer laser. Recently, pioglitazone, an anti-diabetic drug, has shown promising results for some patients.
Non-surgical options like hairpieces, wigs, and hair coloring can help reduce the visibility of hair loss. Hair transplantation is also an option for some patients. Discuss these treatments with your dermatologist to determine the best approach for you.
